Why Are Black Women in America Developing Alzheimer’s Faster Than Anyone Else. And What Does That Reveal About Their Treatment in This Country?
Our brains remember what the system refuses to.
Black women in the United States are developing Alzheimer’s disease at a faster rate and at a younger age than any other demographic group. This is not biology alone; it is the neuropsychological footprint, a term used to describe the unique cognitive and psychological effects of living inside a healthcare system designed to dismiss, delay, and deny care to Black women from birth. The intersecting forces of chronic stress, vascular disease, reproductive trauma, and diagnostic bias have built a perfect storm where cognitive decline is accelerated, yet often ignored. This article unpacks how that happened, what it reveals about the country’s values, and why this crisis demands more than awareness; it requires accountability.
The Urgent Need for Action
The Alzheimer’s Association reports that Black Americans are about twice as likely as white Americans to develop Alzheimer’s or related dementias, and that Black women bear the heaviest burden of all. Epidemiological research confirms that age-adjusted rates of dementia in Black women outpace every other population in the U.S., often beginning 5–10 years earlier.
The Call for Accountability. As Vyas et al. (2023) remind, cardiovascular disease mortality among Black patients remains persistently higher than in their white counterparts, reflecting deeply rooted disparities in access to timely and preventive care. Alzheimer’s doesn’t emerge from nowhere; it grows from the same soil.
The Biological Cost of Chronic Stress
The neuroscience is clear: the brain keeps the score.
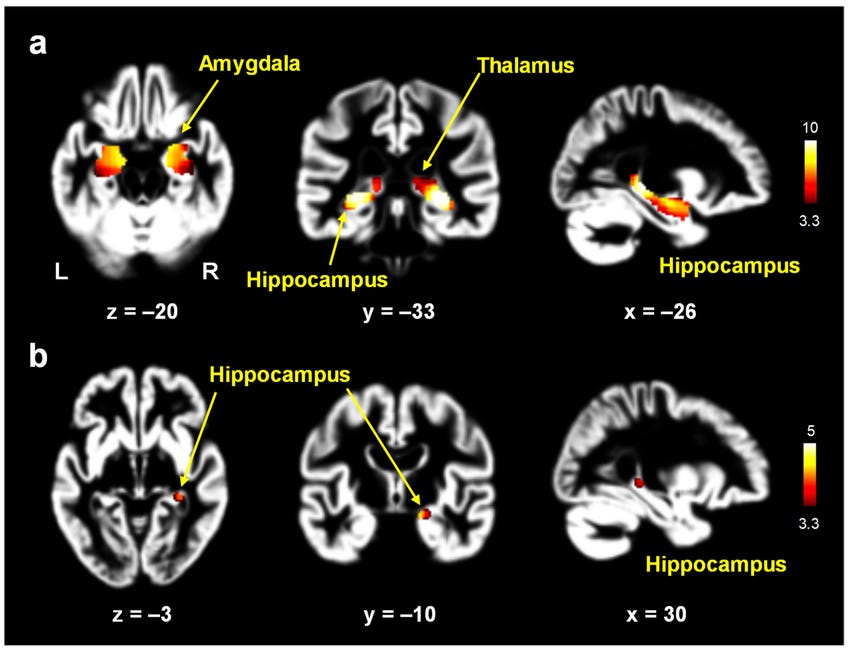
Chronic stress triggers prolonged activation of the hypothalamic–pituitary–adrenal (HPA) axis, keeping cortisol levels high and damaging the hippocampus, the brain’s center for memory and learning.
Research by Balaji et al. (2025) shows that Black women who experience trauma early in life often develop persistent dysregulation of stress systems, a biological echo that extends into adulthood. Williams and Lewis (2019) expand this by showing that gendered racial microaggressions are directly associated with depressive symptoms and physiological stress responses in Black women.
This isn’t about “resilience.” It’s about wearing down. Arline Geronimus called it “weathering” in 1992; the cumulative toll of living in a body that must constantly adapt to hostility. This concept of ‘weathering’ refers to the gradual deterioration of health due to the chronic stress of living in a society characterized by racism and discrimination. Alzheimer’s, in that sense, is the end-stage of chronic disbelief.
Vascular and Reproductive Pathways
Neurodegeneration rarely acts alone. The body’s entire vascular system feeds it.
Hypertension, diabetes, and preeclampsia, conditions that disproportionately affect Black women, are now recognized as major dementia accelerants. The small blood vessels that feed the brain are slowly damaged, starving neurons of oxygen and nutrients.
Vyas et al. (2023) highlight this same vascular vulnerability as a key driver of cardiovascular mortality, while Chung et al. (2024) note elevated hypertensive pregnancy disorders among Black women. These pathologies are not isolated; they’re connected.
The brain doesn’t distinguish between vascular and neurological trauma; it just deteriorates under both.
Diagnostic Bias and the Data Gap
Even when symptoms appear, diagnosis comes late, if at all. Standard neuropsychological assessments are normed on white, middle-class populations. When Black women perform “below average,” clinicians often attribute it to education, effort, or “cultural difference,” not early cognitive decline. By the time Alzheimer’s is officially named, much of the brain tissue has already been lost. Oliveira et al. (2018) described how racial and socioeconomic inequalities drive late-stage cancer diagnoses; the same logic applies here. Structural racism is not just a social condition; it’s a measurable neurological hazard. Chory and Bond (2024) add another layer: inequities in preventive care access persist even in high-resource systems, proving that exclusion is policy, not accident.
Alzheimer’s as a Mirror of National Values
When the fastest-growing form of dementia disproportionately impacts Black women, it says something about what this nation protects, and what it doesn’t. America still treats Black women’s pain as exaggeration, their intellect as expendable, and their health as negotiable. Alzheimer’s exposes those truths on a PET scan. This disease is not just killing memory, it’s indicting the system that forgot us first.
Coming Next (Paid Article Preview)
Next in this series:
When Stress Becomes Structure: How Alzheimer’s Looks in Black Women on a Neuropsychological Level
We’ll examine what chronic stress does to the Black female brain long before diagnosis, mapping how trauma, hypertension, and emotional labor reshape neural networks responsible for memory and regulation. Using psychologist Gary Klein’s “pre-mortem” framework, we’ll explore what prevention looks like before pathology, how to identify, measure, and intervene in the earliest cognitive shifts rather than waiting for decline to confirm what stress already predicted.
References (Zsanine’s format)
Oliveira, M. et al. (2018). Disparidades na mortalidade de câncer colorretal nos estados brasileiros. Revista Brasileira De Epidemiologia.
Vyas, A. et al. (2023). Cardiovascular disease burden and major adverse cardiac events in young Black patients. Journal of the American Heart Association.
Balaji, U. et al. (2025). Social connectedness and well-being among Black women who experienced adolescent sexual trauma. Psychological Trauma.
Williams, M. & Lewis, J. (2019). Gendered racial microaggressions and depressive symptoms among Black women. Psychology of Women Quarterly.
Chung, H. et al. (2024). Season of delivery and risk of hypertensive disorders of pregnancy. Preprint.
Washington, H. A. (2006). Medical Apartheid. Harlem Moon.
Roberts, D. (1997). Killing the Black Body. Vintage.
Cooper Owens, D. (2017). Medical Bondage. University of Georgia Press.
Menakem, R. (2017). My Grandmother’s Hands. Central Recovery Press.
Geronimus, A. T. (1992). “The Weathering Hypothesis.” Ethnicity & Disease.
Morris, M. W. (2016). Pushout: The Criminalization of Black Girls in Schools. The New Press.


Black women are getting Alzheimer’s 5 to 10 years earlier than their counterparts and this is not a coincidence, this is not being studied. With black women being 14% of the population, only 3 to 4% of case studies are us. That means we are not included. And I am referring to black women in the UNITED STATES.
Just recently $45 million worth of funding has “disappeared” regarding the war on our maternal health rates. Do you really think they care about our Alzheimer’s.
This current article taps into why it is important to understand what is going on and how we can address it. Tell me your thoughts.