What Trauma Does to the Pregnant Brain.
It's not just hormones—it's neurological survival. And the science proves it.
During pregnancy, the brain undergoes some of adult life's most dramatic and lasting neurological changes. These shifts are not simply hormonal mood swings or maternal instincts. They are structural transformations, reorganizing regions related to emotion regulation, memory, decision-making, and stress response.
Now, visualize a brain that enters pregnancy already carrying a blueprint of trauma. The blueprint remains intact and gets activated.
I want to hear your story, whether it involves clinical trauma, medical neglect, or ignored mental health during pregnancy. Email me at zsanine@remindlab.org.
Researchers at the NIH found that total brain volume shrinks during pregnancy, particularly in areas that manage emotional processing and social reasoning. These changes aren’t negative—they reflect an intense neurobiological focus on protection, bonding, and regulation. But they also make the brain more sensitive to environmental input, including chronic stress.
“The team found that total brain volume shrank during pregnancy, with changes seen in the size and structure of most large-scale brain networks.”
NIH, 2017
This means a pregnant person’s brain becomes more attuned to perceived threats, social cues, and emotional shifts. When safety and support are present, this sensitivity can enhance bonding. But when trauma is present, the brain may become stuck in survival mode.
When Trauma Collides with Pregnancy
If a pregnant person has a history of trauma, those neurological shifts don’t just reorganize for motherhood—they recalibrate for protection. Hypervigilance becomes a baseline. The nervous system becomes sensitized. And the trauma response—fight, flight, freeze—can begin to operate in the background of every decision, interaction, and internal sensation.
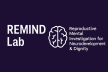
According to a study published in Behavioral Neuroscience (PMC7912216), trauma is linked to changes in the amygdala (which processes fear), the hippocampus (which governs memory), and the prefrontal cortex (which helps regulate emotion and judgment). During pregnancy, these regions are especially plastic, meaning trauma can leave deeper, longer-lasting marks.
That means
Heightened vigilance or anxiety may become constant.
Emotional regulation becomes more difficult, even without external triggers.
Focus, memory, and decision-making can falter under pressure.
Pregnancy isn’t a reset. It’s a neurological amplifier.
And here’s where the story deepens:
If someone was exposed to trauma in childhood, pregnancy may reactivate that stress circuitry.
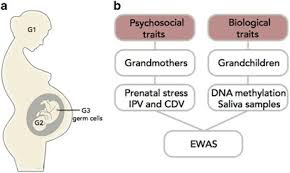
A 2016 study found that unresolved childhood trauma can resurface in pregnancy and influence fetal development via altered cortisol levels and maternal behavior patterns. In short, the stress that shaped you may echo into the life you're carrying.
Trauma doesn’t just shape our past—it can start to structure someone else’s future.
Moog et al., 2016 – PMC4777678
How Trauma Becomes a Blueprint
The NHS outlines how trauma affects the developing brain: fight, flight, or freeze systems become dominant, while areas responsible for empathy, logic, and concentration remain underused. Such experiences can create a lifelong neurological pattern prioritizing survival over reflection and hypervigilance over connection.
Now carry that brain into pregnancy.
What does it mean to build a life inside a nervous system shaped by trauma? What does it mean to nurture while your body is reliving everything that hurt you?
This isn’t just emotional. It’s neurological. And without proper care, it becomes generational.
What This Means for Black Mothers
For Black mothers, many of whom carry compounded trauma from racial violence, systemic neglect, and generational medical mistreatment, these neurological patterns may already be deeply embedded. Pregnancy doesn’t erase them. It activates them.
And yet most providers don’t ask. They don’t screen for trauma. They don’t offer mental health support with the same urgency as physical symptoms. In some cases, they don’t believe us at all.
We are entering pregnancy already coded with survival strategies. Then we give birth in systems built to erase us. What does that do to our brains? What does it do to the children we carry?
To read how this connects directly to the trauma Black mothers face during labor, delivery, and postpartum, continue inside the Lab.
The Black Maternal Brain: A Case for Urgency
Studies show that chronic stress during pregnancy increases the risk of preterm birth, low birth weight, and developmental complications. But for Black mothers, the baseline stress isn’t just individual—it’s systemic.
Microaggressions in clinical care. Provider bias. Dismissed symptoms. The healthcare system views pain thresholds as a matter of race. Living with this kind of stress, and then carrying life within it, isn’t just exhausting. It’s rewiring.
Research published in Obstetrics & Gynecology confirms that Black women are more likely to experience perinatal mood and anxiety disorders but are less likely to be screened or treated for them. Add trauma history, socioeconomic pressure, and medical mistrust, and the brain becomes an active battleground of cortisol, adrenaline, and hypervigilance.
So when we talk about maternal mental health, we cannot afford to treat it like an afterthought. It’s not just a postpartum issue. It’s prenatal. It’s neurological. It’s structural.
We need:
Standardized trauma screening in all prenatal care
Research that centers Black neurobiology and lived experience
Providers trained in trauma-informed and racially conscious care
A record of what we’ve survived—so it can’t be erased
This is why REMIND Lab exists. To document what the system discards. To turn memory into data. To show that this isn’t just about survival—it’s about neurodevelopment, generational outcomes, and structural change.
This is how we fill in what they forgot.
This is REMIND Lab.